All MCAT Biology Resources
Example Questions
Example Question #1 : Types Of Immune System Cells
One component of the immune system is the neutrophil, a professional phagocyte that consumes invading cells. The neutrophil is ferried to the site of infection via the blood as pre-neutrophils, or monocytes, ready to differentiate as needed to defend their host.
In order to leave the blood and migrate to the tissues, where infection is active, the monocyte undergoes a process called diapedesis. Diapedesis is a process of extravasation, where the monocyte leaves the circulation by moving in between endothelial cells, enters the tissue, and matures into a neutrophil.
Diapedesis is mediated by a class of proteins called selectins, present on the monocyte membrane and the endothelium. These selectins interact, attract the monocyte to the endothelium, and allow the monocytes to roll along the endothelium until they are able to complete diapedesis by leaving the vasculature and entering the tissues.
The image below shows monocytes moving in the blood vessel, "rolling" along the vessel wall, and eventually leaving the vessel to migrate to the site of infection.

Neutrophils are best described as being __________.
part of the adaptive immune system
derivatives of B-cells
part of the innate immune system
part of immunological memory
derivatives of natural killer (NK) cells
part of the innate immune system
Neutrophils are one of the main players in innate immunity. Their response does not require having previously been exposed to the pathogen, and they are fairly nonspecific in their ability to digest foreign invaders.
As stated in the passage, neutrophils are derived from monocyctes, not B-cells or natural killer cells.
Example Question #1 : Immune System
Type 1 diabetes is a well-understood autoimmune disease. Autoimmune diseases result from an immune system-mediated attack on one’s own body tissues. In normal development, an organ called the thymus introduces immune cells to the body’s normal proteins. This process is called negative selection, as those immune cells that recognize normal proteins are deleted. If cells evade this process, those that recognize normal proteins enter into circulation, where they can attack body tissues. The thymus is also important for activating T-cells that recognize foreign proteins.
As the figure below shows, immune cells typically originate in the bone marrow. Some immune cells, called T-cells, then go to the thymus for negative selection. Those that survive negative selection, enter into general circulation to fight infection. Other cells, called B-cells, directly enter general circulation from the bone marrow. It is a breakdown in this carefully orchestrated process that leads to autoimmune disease, such as type 1 diabetes.

Di George syndrome is a genetic disorder that results in failure of thymus formation during development, and thus in immune deficiency. A doctor examines the blood of a patient with Di George syndrome. What is she most likely to find?
Excess production of both T-cells and B-cells
A normal complement of both B-cells and T-cells
Deficiency of both T-cells and B-cells
A deficiency of B-cells, with a relative abundance of T-cells
A deficiency of T-cells, with a relative abundance of B-cells
A deficiency of T-cells, with a relative abundance of B-cells
The patient has Di George syndrome, which is characterized by a lack of thymus tissue. Based on the information in the passage, loss of the thymus is most likely to manifest as a deficiency of T-cells, while the presence of B-cells will be relatively unaffected.
Example Question #2 : Immune System
Which answer choice is a part of the adaptive immune response?
Eosinophils
Mast cells
Dendritic cells
Basophils
Neutrophils
Dendritic cells
Adaptive immunity involves specialized cells in response to a specific antigen. When an antigen is detected, it must be presented to the T-cells and B-cells to initiate antibody production. Dendritic cells are involved in this presentation process, and serve as the link between innate and adaptive immunity.
Basophils, eosinophils, neutrophils, and mast cells are specialized granulocytes. Neutrophils help to phagocytose pathogens. Basophils help to repair damaged tissues. Eosinophils and mast cells are both involved in mediating the inflammatory response.
Example Question #1 : Types Of Immune System Cells
When heart surgeries were initially performed on children, surgeons would sometimes discard the thymus because they did not know its function. These children would often die due to which lost function of the thymus?
T3 and T4 levels would decrease
B-cells would not be able to mature
T-cells could not be generated
Hypothyroidism would occur
T-cells would not be able to mature
T-cells would not be able to mature
The correct answer is that T-cells would not be able to mature. Both T-cells and B-cells are generated in the bone marrow, however, their sites of maturation are different. B-cells mature in the bone marrow, whereas T-cells mature in the thymus.
T3 and T4 are thyroid hormones, and are unlinked to the thymus. Hypothyroidism occurs due to a deficiency in these hormones.
Example Question #4 : Immune System
Duchenne Muscular Dystrophy is an X-linked recessive genetic disorder, resulting in the loss of the dystrophin protein. In healthy muscle, dystrophin localizes to the sarcolemma and helps anchor the muscle fiber to the basal lamina. The loss of this protein results in progressive muscle weakness, and eventually death.
In the muscle fibers, the effects of the disease can be exacerbated by auto-immune interference. Weakness of the sarcolemma leads to damage and tears in the membrane. The body’s immune system recognizes the damage and attempts to repair it. However, since the damage exists as a chronic condition, leukocytes begin to present the damaged protein fragments as antigens, stimulating a targeted attack on the damaged parts of the muscle fiber. The attack causes inflammation, fibrosis, and necrosis, further weakening the muscle.
Studies have shown that despite the severe pathology of the muscle fibers, the innervation of the muscle is unaffected.
Which of the following does not play a key role in the adaptive immune response?
helper T-cells
cytotoxic T-cells
dendritic cells
natural Killer cells
B-cells
natural Killer cells
The adaptive immune response involves the presentation of antigens, identification of antigens, activation of immune response, and elimination of pathogens. Dendritic cells present the antigen to the helper T-cells, which identify it and activate B-cells and cytotoxic T-cells to eliminate the pathogen.
Natural killer cells play a key role in the innate immune response by eliminating pathogens without the recognition of antigens.
Example Question #5 : Immune System
Sexually transmitted diseases are a common problem among young people in the United States. One of the more common diseases is caused by the bacterium Neisseria gonorrhoeae, which leads to inflammation and purulent discharge in the male and female reproductive tracts.
The bacterium has a number of systems to evade host defenses. Upon infection, it uses pili to adhere to host epithelium. The bacterium also uses an enzyme, gonococcal sialyltransferase, to transfer a sialyic acid residue to a gonococcal surface lipooligosaccharide (LOS). A depiction of this can be seen in Figure 1. The sialyic acid residue mimics the protective capsule found on other bacterial species.
Once infection is established, Neisseria preferentially infects columnar epithelial cells in the female reproductive tract, and leads to a loss of cilia on these cells. Damage to the reproductive tract can result in pelvic inflammatory disease, which can complicate pregnancies later in the life of the woman.

A key immune response to Neisseria in humans is the activity of macrophages. What is true of how macrophages combat infection?
Macrophages only recruit other cells that are then able to kill pathogens
Macrophages produce antibodies to target pathogens
Macrophages use reactive oxygen species after ingesting pathogens
Macrophages undergo apoptosis and release toxic compounds
Macrophages use isolation as their main defense, and wall off pathogens
Macrophages use reactive oxygen species after ingesting pathogens
Macrophages are professional phagocytic cells. They ingest pathogens, and often use reactive oxygen species to kill pathogens via a burst of radical activity in specialized cellular compartments.
Example Question #6 : Immune System
Scientists use a process called Flourescent In-Situ Hybridization, or FISH, to study genetic disorders in humans. FISH is a technique that uses spectrographic analysis to determine the presence or absence, as well as the relative abundance, of genetic material in human cells.
To use FISH, scientists apply fluorescently-labeled bits of DNA of a known color, called probes, to samples of test DNA. These probes anneal to the sample DNA, and scientists can read the colors that result using laboratory equipment. One common use of FISH is to determine the presence of extra DNA in conditions of aneuploidy, a state in which a human cell has an abnormal number of chromosomes. Chromosomes are collections of DNA, the totality of which makes up a cell’s genome. Another typical use is in the study of cancer cells, where scientists use FISH labels to ascertain if genes have moved inappropriately in a cell’s genome.
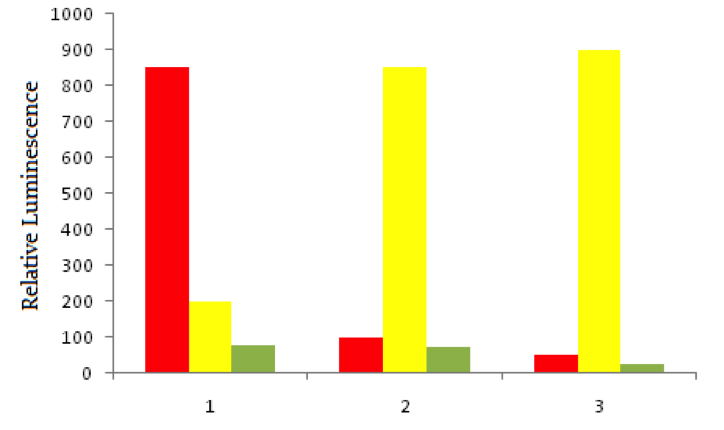
Using red fluorescent tags, scientists label probe DNA for a gene known to be expressed more heavily in cancer cells than normal cells. They then label a probe for an immediately adjacent DNA sequence with a green fluorescent tag. Both probes are then added to three dishes, shown below. In dish 1 human bladder cells are incubated with the probes, in dish 2 human epithelial cells are incubated, and in dish 3 known non-cancerous cells are used. The relative luminescence observed in regions of interest in all dishes is shown below.
When the body recognizes that cells have become cancerous, it responds in part by mobilizing cell-mediated killing of cancer cells. What cells are most likely responsible for this killing?
CD8+ T-cells
B-cells
CD4+ T-cells
Macrophages
Plasma cells
CD8+ T-cells
CD8+ T-cells are also called cytotoxic T-cells. They are the main agents of cell-mediated immune cytotoxicity. This function is critical for the elimination of virally infected or cancerous cells. Macrophages, in contrast, are responsible for eliminating foreign pathogens and do not attack non-foreign cells.
Example Question #2 : Immune System
Where do the T-cells of the immune system mature into functional T-cells?
Bone marrow
Spleen
Thymus
Lymph nodes
Thymus
T-cells are originally formed from stem cells in the bone marrow, however, T-cells, unlike B-cells, mature in the thymus. The thymus is a lymphoid organ located in the upper chest.
In contrast, B-cells are formed and mature in the bone marrow.
Example Question #1 : Types Of Immune System Cells
Which of the following is NOT an antigen presenting cell?
Macrophages
Dendritic cells
T-Cells
B-Cells
T-Cells
This question asks which of the following is NOT an antigen presenting cell, therefore, any option that is an antigen presenting cell in the immune system is an INCORRECT answer.
During an immune response, the cells involved in antigen presentation are dendritic cells, macrophages, and B-cells. T-cells, then, must be the answer choice that is NOT an antigen presenting cell, and thus is the correct answer.
Example Question #10 : Immune System
Most scientists subscribe to the theory of endosymbiosis to explain the presence of mitochondria in eukaryotic cells. According to the theory of endosymbiosis, early pre-eukaryotic cells phagocytosed free living prokaryotes, but failed to digest them. As a result, these prokaryotes remained in residence in the pre-eukaryotes, and continued to generate energy. The host cells were able to use this energy to gain a selective advantage over their competitors, and eventually the energy-producing prokaryotes became mitochondria.
In many ways, mitochondria are different from other cellular organelles, and these differences puzzled scientists for many years. The theory of endosymbiosis concisely explains a number of these observations about mitochondria. Perhaps most of all, the theory explains why aerobic metabolism is entirely limited to this one organelle, while other kinds of metabolism are more distributed in the cellular cytosol.
Some version of phagocytosis was likely the initial event that introduced a free-living prokaryote into the host described in the passage. Which of the following cells is most commonly associated with phagocytosis?
Endothelial cell
Lymphocyte
Neuron
Myocyte
Neutrophil
Neutrophil
Neutrophils are professional phagocytes of the immune system. They prevent infection by phagocytosing potential invaders.
Note, however, that neutrophils could not have been the initial cell type to phagocytose a free-living prokaryote. Neutrophils are eukaryotic, and evolved long after endosymbiosis first occurred. They are, however, still closely linked to phagocytosis in humans.
Certified Tutor
Certified Tutor
All MCAT Biology Resources



