All MCAT Biology Resources
Example Questions
Example Question #52 : Immune And Lymphatic Systems
Which of the following cells would be categorized as an agranulocyte?
Neutrophil
Monocyte
Basophil
Eosinophil
Monocyte
Granulocytes are cells categorized because they have vesicles within their membrane that look similar to a granule. Basophils, eosinophils and neutrophils all present granule-like figures and are categorized as granulocytes. Although they derive from the same myeloid stem cells as the granulocytes, monocytes are categorized as agranulocytes.
Example Question #32 : Immune System
Which of the following molecules is not associated with the function of cytotoxic T-cells?
MHC I
Cytokines
MHC II
CD8
MHC II
In terms of MHC restriction, students should be familiar with the fact that cytotoxic T-cells are CD8+ and MHC I restricted. The alternative T subset, the helperT-ell, is CD4+ and MHC II restricted. Both cells rely on cytokines for growth, survival, and their effector functions.
Example Question #31 : Types Of Immune System Cells
Eosinophils are play a multi-facted role in the innate immune response especially against parasites. They have been shown to phagocytose different parasites, release cytotoxic granule proteins such as major basic protein (MBP), present antigens to T cells, and produce several different cytokines to promote the inflammatory process.
Eosinophils play a critical role in innate and adaptive immune response against parasitic infections. Which of the following is not a function of eosinophils?
Release of cytotoxic granule proteins
Phagocytosis
Antigen presentation
Antibody production
Production of cytokines
Antibody production
Eosinophils are unable to produce antibody, which are limited to the B cell lineage.
Example Question #32 : Types Of Immune System Cells
What is the difference between helper T cells and cytotoxic T cells?
Helper T cells express CD4 while cytotoxic T cells express CD8.
Helper T cells express MHC II while cytotoxic T cells express MHC I.
Cytotoxic T cells directly kill pathogens while helper T cells assist other immune cells in the inflammatory response.
Helper T cells are more adept at cytokine production.
All of these
All of these
Generally, cytotoxic T cells express CD8, express MHC I, are adept at killing specific targets, and while they can produce some cytokines, helper T cells predominantly secrete more different kinds of cytokines and larger quantities of cytokines. Helper T cells express CD4, MHC II, and function primarily in producing cytokines to activate and induce other immune cells to function in the inflammatory response.
Example Question #373 : Systems Biology And Tissue Types
Which of these choices is not a function of T-cells?
Increase the activity of immune cells (such as B-cells and macrophages) through the release of chemical messengers
Directly produce antibodies after the first response to an antigen
Inhibit the activity of both B- and T-cells
Locate and kill cells that contain antigens bound to MHC-I proteins
Secrete cytokines
Directly produce antibodies after the first response to an antigen
The only choice that is not a function of any type of T-cell is the direct production of antibodies (which is performed by B-cells). Cytotoxic T-cells kill other cells that are bound to antigen/MHC-I complexes. Suppressor T-cells tone down the response of both B- and T-cells, and helper T-cells secrete cytokines, which increase the activity of many other immune cell types.
Example Question #32 : Immune System
Sexually transmitted diseases are a common problem among young people in the United States. One of the more common diseases is caused by the bacterium Neisseria gonorrhoeae, which leads to inflammation and purulent discharge in the male and female reproductive tracts.
The bacterium has a number of systems to evade host defenses. Upon infection, it uses pili to adhere to host epithelium. The bacterium also uses an enzyme, gonococcal sialyltransferase, to transfer a sialyic acid residue to a gonococcal surface lipooligosaccharide (LOS). A depiction of this can be seen in Figure 1. The sialyic acid residue mimics the protective capsule found on other bacterial species.
Once infection is established, Neisseria preferentially infects columnar epithelial cells in the female reproductive tract, and leads to a loss of cilia on these cells. Damage to the reproductive tract can result in pelvic inflammatory disease, which can complicate pregnancies later in the life of the woman.

The first line of defense by a human host against a potential Neisseria infection is which of the following?
Cytotoxic defense
Lymphocyte-mediated defense
Genetic immunity
Antibody defense
Innate immune defense
Innate immune defense
Innate defenses, such as the skin or macrophages, are the first line of defense against infection. Other responses only become effective if a pathogen cannot be repelled by innate mechanisms.
Example Question #32 : Immune System
Which of the following is not an example of innate immunity?
Histamine release by mast cells
Degradation of bacterial cell walls by saliva
Removal of bacterial organisms by cilia
Antibody production by B-cells
Antibody production by B-cells
All of the following are examples of non-specific defense mechanisms of the immune system, except for antibody production by B-cells. B-cells respond to specific antigens within the body via immunoglobulins located on the plasma membrane of B-cells. This type of response is known as adaptive immunity, and develops only after a particular pathogen has invaded the immune system.
Example Question #33 : Immune System
Which of the following is not a component of innate immunity?
Macrophages
Plasma cells
Stomach acid
Mast cells
Plasma cells
The innate immune system defends against pathogens, even without identifying what the pathogens are. Innate immunity includes physical and chemical barriers, such as the skin and stomach acid, which can kill some bacteria or prevent their entry into the body. Macrophages are responsible for phagocytosis of foreign pathogens without antibody mediation. Mast cells release histamine in response to infection or injury. Plasma cells, however, are mature B-cells that secrete antibodies in response to initiation of the adaptive immune response.
Example Question #35 : Immune System
Hypersensitivity reactions occur when body tissues are affected by an abnormal immune reaction. The result is damage to normal tissues and clinical illness. A peanut allergy is an example of a hypersensitivity reaction, but there are three additional broad classes.
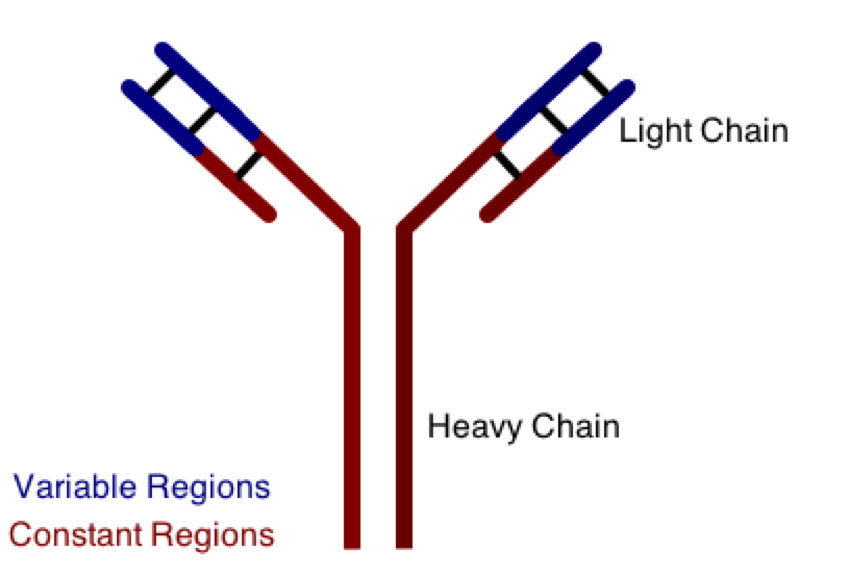
One class involves the abnormal production or deposition of antibodies. Antibodies are B-cell derived molecules that normally adhere to pathogens, rendering them unable to continue an infection. When antibodies are produced against normal tissues, however, disease can result. Figure 1 depicts a schematic structure of an antibody.
Antibodies can be divided into two peptide chains: heavy and light. Heavy chains form the backbone of the antibody, and are attached to light chains via covalent bonding. Each heavy and light chain is then further divided into constant and variable regions. Variable regions exhibit molecular variety, generating a unique chemical identity for each antibody. These unique patterns help guarantee that the body can produce antibodies to recognize many possible molecular patterns on invading pathogens.
An antibody response is similar to an inflammatory response in that:
I. They are both innate immune responses
II. They are both most effective immediately following the first infection with a pathogen
III. They are both dependent on chemical mediators, such as cytokines, for function
I and II
I, II, and III
I and III
III only
II only
III only
Cytokines are important immune mediators, and are components of both adaptive and innate immunity. B- and T-lymphocytes are mediators of adaptive immunity, while inflammation is a non-specific innate immune response to a pathogen. While innate immunity, such as the inflammatory response, is active immediately following an infection, adaptive immunity requires a previous exposure to the pathogen to become most effective. The body must already recognize the invading antigen in order to activate the antibody response.
Statement I is false, statement II is false, and statement III is true.
Example Question #31 : Immune System
Duchenne Muscular Dystrophy is an X-linked recessive genetic disorder, resulting in the loss of the dystrophin protein. In healthy muscle, dystrophin localizes to the sarcolemma and helps anchor the muscle fiber to the basal lamina. The loss of this protein results in progressive muscle weakness, and eventually death.
In the muscle fibers, the effects of the disease can be exacerbated by auto-immune interference. Weakness of the sarcolemma leads to damage and tears in the membrane. The body’s immune system recognizes the damage and attempts to repair it. However, since the damage exists as a chronic condition, leukocytes begin to present the damaged protein fragments as antigens, stimulating a targeted attack on the damaged parts of the muscle fiber. The attack causes inflammation, fibrosis, and necrosis, further weakening the muscle.
Studies have shown that despite the severe pathology of the muscle fibers, the innervation of the muscle is unaffected.
Which compound is most likely responsible for initiating the inflammation response that results from the autoimmune attack?
Fibrogen
Dopamine
Fibrinogen
Fibrin
Histamine
Histamine
Fibrin and fibrinogen are involved in wound healing and scab formation. Dopamine is a neurotransmitter in the brain. Fibrogen is not a real protein at all.
Histamine is the primary inflammatory molecule in the body and is released from mast cells during an immune response or trauma.
Certified Tutor
Certified Tutor
All MCAT Biology Resources




